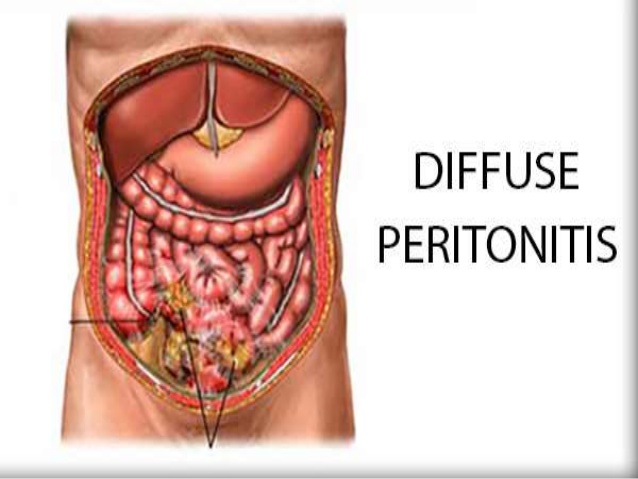
You have a thin layer of tissue covering the inside of your abdomen and most of its organs. This is called the peritoneum. Peritonitis is inflammation of the peritoneum. The inflammation is usually the result of a fungal or bacterial infection caused by an abdominal injury, an underlying medical condition, or a treatment device, such as a dialysis catheter or feeding tube.Peritonitis is a serious condition that needs immediate medical attention. Prompt intravenousantibiotics are needed to treat the infection. Surgery is sometimes necessary to remove infected tissue. The infection can spread and become life-threatening if it isn’t treated promptly.
What Causes Peritonitis?
There are two types of peritonitis. Spontaneous bacterial peritonitis (SBP) is the result of an infection of the fluid in your peritoneal cavity. Liver or kidney failure can cause this condition. People on peritoneal dialysis for kidney failure are also at increased risk for SBP.
Secondary peritonitis is usually due to an infection that has spread from your digestive tract.
The following conditions can lead to peritonitis:
- an abdominal wound or injury
- a ruptured appendix
- a stomach ulcer
- a perforated colon
- diverticulitis, which is when pouches form on the wall of the colon and become inflamed
- pancreatitis, which is an inflammation of the pancreas
- cirrhosis of the liver or other types of liver disease
- infection of the gallbladder, intestines, or bloodstream
- pelvic inflammatory disease, which is an infection of a woman’s reproductive organs
- Crohn’s disease, which is a type of inflammatory bowel disease
- invasive medical procedures, including treatment for kidney failure, surgery, or the use of a feeding tube
Symptoms of Peritonitis
Symptoms will vary depending on the underlying cause of your infection. Common symptoms of peritonitis include:
- tenderness in your abdomen
- pain in your abdomen that gets more intense with motion or touch
- abdominal bloating or distention
- nausea and vomiting
- diarrhea
- constipation or the inability to pass gas
- minimal urine output
- anorexia, or loss of appetite
- excessive thirst
- fatigue
- fever and chills
If you’re on peritoneal dialysis, your dialysis fluid may appear cloudy or have white flecks or clumps in it. You may also notice redness or feel pain around your catheter.
Diagnosing Peritonitis
If you have symptoms of peritonitis, seek medical attention right away. Delaying your treatment could put your life at risk.
Your doctor will ask you about your medical history and perform a complete physical exam. This will include touching or pressing on your abdomen, which will probably cause some discomfort.
There are other tests to help diagnose peritonitis:
- A blood test, called a complete blood count (CBC) can measure your white blood cell count. A high white blood cell count usually signals inflammation or infection. A blood culture can help to identify the bacteria causing the infection or inflammation.
- If you have a buildup of fluid in your abdomen, your doctor can use a needle to remove some and send it to a laboratory for fluid analysis. Culturing the fluid can also help identify bacteria.
- Imaging tests, such as CT scans and X-rays, can show any perforations or holes in your peritoneum.
If you’re on dialysis, your doctor may diagnose you based on the appearance of cloudy dialysis fluid.
How Peritonitis Is Treated
The first step in treating peritonitis is determining its underlying cause. Treatment usually involves antibiotics to fight infection and medication for pain.
If you have infected bowels, an abscess (a collection of pus), or an inflamed appendix, you may need surgery to remove the infected tissue.
If you’re on kidney dialysis and have peritonitis, you may have to wait until the infection clears up to receive more dialysis. If the infection continues, you might need to switch to a different type of dialysis.
Your treatment must begin promptly to avoid serious and potentially fatal complications.
Complications from Peritonitis
If it’s not treated promptly, the infection may enter your bloodstream, causing shock and damage to your other organs. This can be fatal.
The potential complications of spontaneous peritonitis include:
- hepatic encephalopathy, which is a loss of brain function that occurs when the liver can no longer remove toxic substances from your blood
- hepatorenal syndrome, which is progressive kidney failure
- sepsis, which is a severe reaction that occurs when the bloodstream becomes overwhelmed by bacteria
The complications of secondary peritonitis include:
- an intra-abdominal abscess, which is a collection of pus
- gangrenous bowel, which is dead bowel tissue
- intraperitoneal adhesions, which are bands of fibrous tissue that join abdominal organs and can cause bowel blockage
- septic shock, which is characterized by dangerously low blood pressure
How to Prevent Peritonitis
If you’re on dialysis, wash your hands and fingernails before touching your catheter. Clean the skin around the catheter daily. Follow your doctor’s instructions regarding the care and storage of your medical supplies.
See your doctor, go to an emergency room, or call 911 if you have severe abdominal pain or an abdominal injury, such as a knife wound.
Long-Term Outlook for Peritonitis
The outlook for peritonitis depends on the cause of your infection and how far it had progressed before treatment began. Medications and surgery are usually able to bring the infection under control.
If treatment doesn’t begin early, the infection can spread. If other organs are damaged, your recovery will depend on your overall health and how much damage was done.