Crohn's shares symptoms with diseases like ulcerative colitis, making it difficult to diagnose. Gut inflammation triggers diarrhea, lower abdominal pain, bowel incontinence, constipation, ulcers, anal fissures, fever, fatigue, anemia, and malnutrition. Stress and low-fiber diets worsen the condition. Immunosuppressants and nutrient supplements provide relief to Crohn's patients.
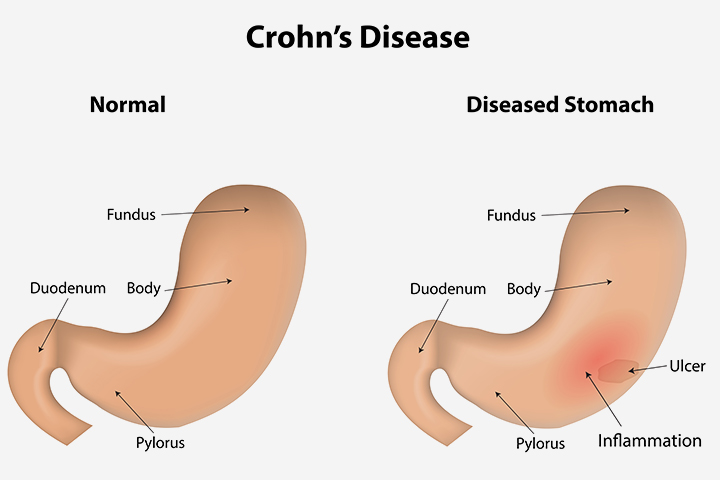
With symptoms like abdominal pain, diarrhea, and general malaise, Crohn’s disease is one of the most common inflammatory bowel disorders (IBDs). Named after Dr. Burrill B. Crohn, who with his colleagues discovered the disease in 1932, Crohn’s is a chronic inflammatory disorder of the gastrointestinal tract (mostly the gut). It can affect any part of the gut and symptoms tend to flare up from time to time.
Incidence And Prevalence
Crohn’s affects 1 in 10,000 people each year. It usually begins to show up anywhere between the age of 15 to 30 and affects women more than men. Crohn’s disease is most common in developed, urban regions and is also known to occur more among white people of European descent, especially descendants of the Ashkenazi Jews. Possible triggers include a combination of hereditary genes, lifestyle (excess smoking, alcohol, high-fat diet with little roughage, abnormal reaction of the immune system in response to bacteria in the intestine, and other triggers like stress), and unknown immune reactions. One study found that signs and symptoms of Crohn’s can be exacerbated by stress.
Diagnostic Issues
Crohn’s is not easily diagnosed as the symptoms tend to be mistaken for other digestive disorders like ulcerative colitis, enteric infection and abscess, bacterial overgrowth, bile salt malabsorption, dysmotility (IBS), or gall stones. Any suspicion of Crohn’s must be referred to a gastroenterologist who will take a full history and physical along with current symptoms to arrive at a clinical diagnosis. This will be correlated with laboratory and radiology tests.
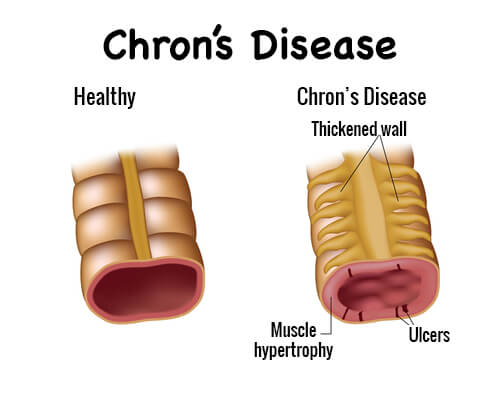
Symptoms
A person with Crohn’s will usually present with the following symptoms as a result of the inflamed gut.
Pain is the most common symptom. In Crohn’s, the small intestine or ileum is most commonly affected and therefore the pain arises in the right side of the lower abdomen. This pain is often mistaken for appendicitis, which should be ruled out too. The type and severity of the pain vary and each individual feels it differently. It could be a dull to intense pain, moderate to extreme. For a person already diagnosed with Crohn’s, a sudden onset of severe pain could be a sign of complications that need immediate medical attention.
Urgent need to pass bowels is another symptom which occurs in 7 out of 10 people diagnosed with Crohn’s. This can come on suddenly accompanied by dull pain. Also one of the more irritating symptoms, this causes a lot of distress to people with Crohn’s. A feeling of incomplete evacuation of bowels is also common in this case, which in turn causes residual pain and irritation.
Constipation is another symptom frequently plaguing Crohn’s sufferers. This can often lead to obstructive bowel disorders which may require treatment and even procedures like bowel decompression or surgery
Diarrhea is a recurrent symptom of Crohn’s and often a disabling symptom that interferes with daily life. It can vary from mild to severe with pain. Blood and mucus may often be present.
Ulcers which often occur within the gut, sometimes in the mouth, are common. A bleeding gut ulcer is indicated when stools are tinged with blood.
Anal fissures occur because a person with Crohn’s is often forced to evacuate bowels frequently. This can cause bleeding.
Weight loss, anemia, and malnutrition are common symptoms because Crohn’s sufferers often have a poor appetite and cannot keep food down properly. Weight loss is often accompanied by anemia and malnutrition. Anemia occurs because of loss of blood and insufficient nutrition.
Fever and fatigue are other common symptoms. Fever is a fallout of any inflammatory disorder while the fatigue too is a result of the physical stress of the body dealing with a chronic inflammatory state.
Diagnosis
The presence of these symptoms can help confirm a clinical diagnosis of Crohn’s. However, your doctor will ask for a range of lab and imaging tests to confirm. Blood tests will include complete blood counts, platelet counts, erythrocyte sedimentation rate, C reactive protein, and serum albumin. Other imaging and investigative procedures include barium x-rays of the GI tract, upper endoscopy, colonoscopy, and small intestine imaging through Computed Tomography (CT) scan or Magnetic Resonance Imaging (MRI)
Treatment
Treatment for Crohn’s includes steroids to suppress the immune system especially during flareups; immunosuppressants to modify the immune system; a course of antibiotics to deal with gastrointestinal infections; aminosalicylates (compounds containing 5-amino salicylic acid) to reduce inflammation in the lining of the intestine); nutritional support and supplements; and in some cases surgery (to remove severely affected parts of the gut)
Treatment often provides remission for a certain period of time. But Crohn’s is a chronic disease and you might have to deal with it throughout your life. There may be periods when the symptoms subside and normal life is possible.
At present, there is no cure for Crohn’s. The best way to manage Crohn’s is with symptom management along with the right diet, nutrition, exercise, and positive lifestyle (e.g., quitting smoking and alcohol). Each person should make a list of what foods trigger symptoms and avoid these. Avoiding emotional stress and staying positive are also important.